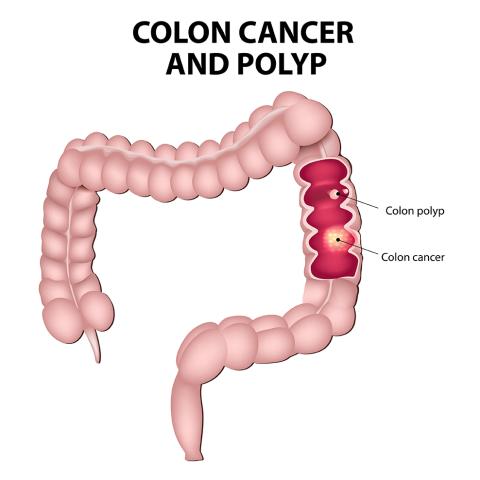
Colorectal cancer, also known as colon cancer or rectal cancer, refers to cancer that develops in the colon (large intestine) or rectum. It is one of the most common types of cancer worldwide, with significant morbidity and mortality rates. Colorectal cancer typically develops from precancerous polyps (abnormal growths) in the colon or rectum, which can evolve into cancer over time if left untreated.
Risk Factors: Several risk factors may increase the likelihood of developing colorectal cancer. These include age (risk increases with age, particularly after age 50), family history of colorectal cancer or polyps, personal history of inflammatory bowel disease (such as Crohn’s disease or ulcerative colitis), certain genetic syndromes (such as familial adenomatous polyposis or Lynch syndrome), unhealthy lifestyle factors (such as high consumption of red or processed meats, low intake of fruits and vegetables, lack of physical activity, obesity, smoking, and heavy alcohol use), and racial and ethnic background.
Symptoms: Symptoms of colorectal cancer may vary depending on the location and stage of the cancer. Common symptoms may include changes in bowel habits (such as diarrhea, constipation, or narrowing of the stool), rectal bleeding or blood in the stool, persistent abdominal discomfort (such as cramps, gas, or pain), unexplained weight loss, weakness, fatigue, and a feeling that the bowel does not empty completely. However, not all colorectal cancers cause symptoms, especially in the early stages.
Screening: Screening for colorectal cancer aims to detect precancerous polyps or early-stage cancer when treatment is most effective. Screening methods include stool-based tests (such as fecal occult blood tests or stool DNA tests) and visual exams (such as colonoscopy, flexible sigmoidoscopy, or virtual colonoscopy). The choice of screening method and frequency may depend on factors such as age, family history, personal risk factors, and individual preferences.
Diagnosis: Colorectal cancer is typically diagnosed through a combination of methods, including screening tests, diagnostic imaging (such as colonoscopy, CT scan, or MRI), and biopsy (removal and examination of a sample of tissue from the colon or rectum). The biopsy helps determine the presence of cancer cells and the specific characteristics of the tumor, which are important for treatment planning.
Treatment: Treatment for colorectal cancer depends on factors such as the stage of the cancer, the location and size of the tumor, the individual’s overall health and preferences, and potential side effects of treatment. Treatment options may include surgery (such as removal of the tumor or part of the colon or rectum), chemotherapy, radiation therapy, targeted therapy, immunotherapy, and adjuvant therapy (additional treatment after primary therapy to lower the risk of cancer recurrence).
Prognosis: The prognosis for colorectal cancer varies depending on factors such as the stage of the cancer, the presence of specific genetic mutations or biomarkers, and how well the cancer responds to treatment. Colorectal cancer diagnosed at an early stage (before it has spread beyond the colon or rectum) generally has a better prognosis, with higher survival rates.
Prevention: Several lifestyle modifications and preventive measures may help reduce the risk of developing colorectal cancer, including maintaining a healthy diet high in fruits, vegetables, and whole grains; limiting consumption of red and processed meats; being physically active; maintaining a healthy weight; avoiding smoking; limiting alcohol consumption; and undergoing regular colorectal cancer screening as recommended by healthcare providers.



