Immunotherapy is a type of cancer treatment that harnesses the body’s own immune system to recognize, target, and destroy cancer cells. Unlike traditional cancer treatments such as chemotherapy, which directly kill cancer cells, immunotherapy works by boosting the body’s natural defenses against cancer, enabling the immune system to more effectively recognize and attack cancer cells.
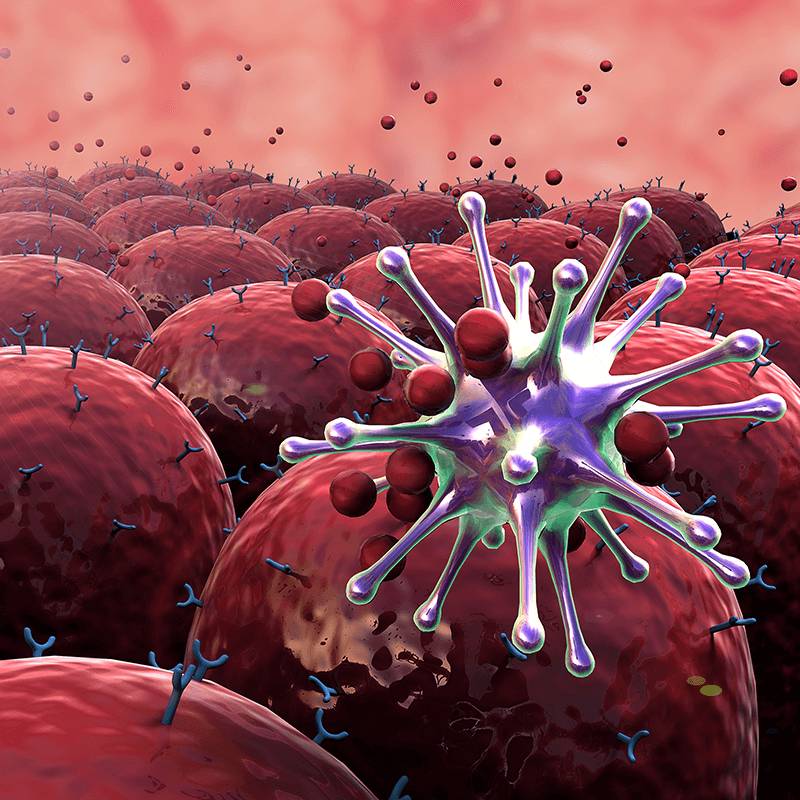
Mechanism of Action: Immunotherapy works by stimulating or enhancing the body’s immune response against cancer. Cancer cells can evade detection by the immune system through various mechanisms, such as suppressing immune responses or expressing proteins that inhibit immune cell activity. Immunotherapy drugs target these mechanisms, allowing the immune system to recognize and attack cancer cells more effectively. There are several types of immunotherapy, each with its own mechanism of action:
- Checkpoint inhibitors: These drugs block proteins called checkpoint molecules, such as PD-1, PD-L1, and CTLA-4, which normally act as “brakes” on the immune system’s response. By blocking these checkpoints, checkpoint inhibitors release the brakes and allow immune cells to attack cancer cells more effectively.
- Monoclonal antibodies: These are antibodies that are designed to recognize and bind to specific proteins on the surface of cancer cells, marking them for destruction by the immune system or triggering an immune response against them.
- Adoptive cell therapy: This approach involves extracting immune cells from the patient, modifying them to enhance their cancer-fighting abilities (such as engineering them to express chimeric antigen receptors, or CARs), and infusing them back into the patient to target and kill cancer cells.
- Cancer vaccines: These vaccines are designed to stimulate the immune system to recognize and attack cancer cells by presenting tumor-specific antigens or fragments of cancer cells to immune cells, triggering an immune response against the cancer.
Indications: Immunotherapy has been approved for the treatment of various types of cancer, including melanoma, lung cancer, kidney cancer, bladder cancer, head and neck cancer, Hodgkin lymphoma, non-Hodgkin lymphoma, and certain types of leukemia. The choice of immunotherapy depends on factors such as the type and stage of cancer, the specific molecular characteristics of the tumor, and the individual’s overall health and treatment goals.
Treatment Approach: Immunotherapy may be used alone or in combination with other cancer treatments such as chemotherapy, radiation therapy, targeted therapy, or other immunotherapy drugs, depending on the specific characteristics of the cancer and the treatment plan. Combination therapies may be more effective in some cases by targeting multiple pathways involved in cancer growth and progression.
Side Effects: Immunotherapy can cause side effects by stimulating the immune system to attack cancer cells as well as normal cells and tissues. Common side effects of immunotherapy may include fatigue, skin rash, diarrhea, nausea, fever, flu-like symptoms, and inflammation of organs such as the lungs, liver, or thyroid. These side effects are generally less severe than those of traditional chemotherapy, but they can still impact quality of life and may require supportive care measures or dose adjustments.
Response and Resistance: Immunotherapy can lead to durable responses and long-term remission in some patients, but not all patients respond to treatment, and some may develop resistance over time. Factors that may influence response to immunotherapy include the type and stage of cancer, the presence of specific molecular markers or mutations, the overall health of the patient’s immune system, and the tumor microenvironment. Ongoing research is focused on identifying biomarkers and developing strategies to overcome resistance to immunotherapy.



